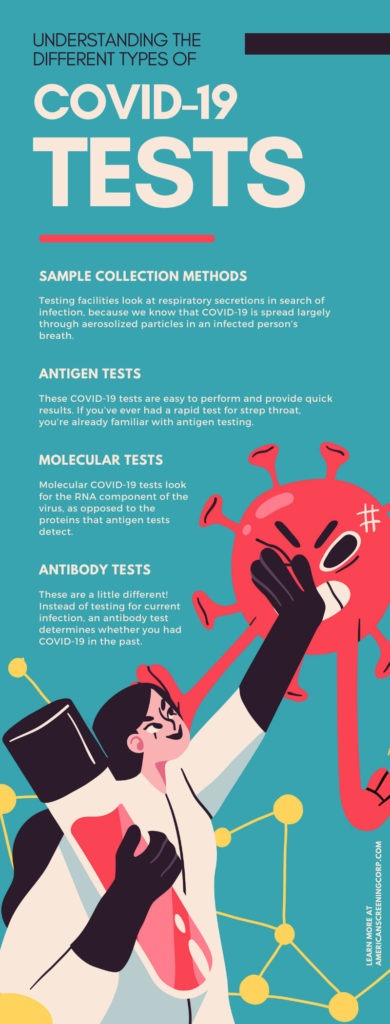
Understanding the Different Types of COVID-19 Tests
Over the past two years, the American public has had an extended science lesson. What is social distancing? How do masks and other PPE help stop the spread of COVID-19? Effective and accessible COVID-19 testing also helps inform the public about their status to make important health decisions. In order to speed the ending of the pandemic, we must continue regular testing. But what kinds of tests are out there? Scientists have been working at breakneck speed for the past two years, creating tests and vaccines that will help slow the spread. Let’s look at a few different tests. Understand the different types of COVID-19 tests and choose the one that is right for you.
Sample Collection Methods
If you’ve been tested for COVID-19, you may have had a very long, thin swab inserted far up your nose. That’s called a nasopharyngeal swab; experts have found this collection method to be remarkably effective. Other tests will simply use a nasal swab without reaching far up into your sinuses. The third swab collection method targets the very back of your throat, called an oropharyngeal swab. It may be an uncomfortable experience; with the nasopharyngeal swab, your eyes will water if the test is performed correctly. The oropharyngeal swab may trigger your gag reflex. But it only lasts for a few seconds, and the results are remarkably effective.
Currently, these are the main collection methods. Testing facilities look at respiratory secretions in search of infection, because we know that COVID-19 is spread largely through aerosolized particles in an infected person’s breath. Experts are looking at the possibility of saliva testing, which would be less invasive than the swab. Early data has suggested that infected cells can be detected in saliva just as well as in respiratory secretions in the sinuses.
Antigen Tests
These COVID-19 tests are easy to perform and provide quick results. If you’ve ever had a rapid test for strep throat, you’re already familiar with antigen testing. Public health officials are interested in testing large populations of people to screen for COVID-19 and identify viral hot spots. Schools in particular have been looking at antigen tests as a way to test a whole group of students at once.
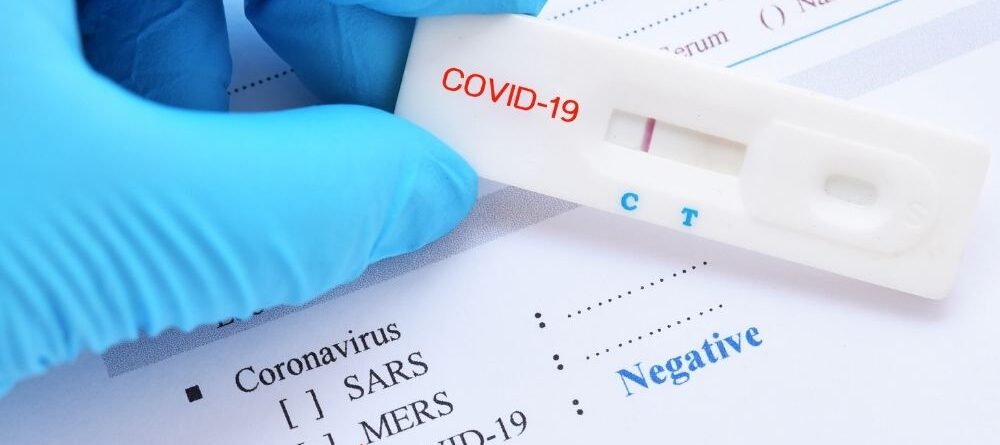
Antigen tests look for the presence of viral proteins in the subject’s upper respiratory sample, generally collected via a nasopharyngeal swab. The nucleocapsid (N) protein that carries the virus latches onto healthy cells, and an antigen test looks for the presence of that N protein. The sample is mixed with a reagent, and the resulting liquid is gently dripped onto a testing card. Different sections of that testing card are covered with different antibodies that bind to that N protein. If those viral particles inside the N protein are present in the sample, they’ll latch onto a specific location on the test strip. The tester will see a colored line present on the testing strip and determine the presence of those viral particles.
The rapid antigen test has been popular during this pandemic, due to its ease of sample collection and quick responses. However, with that convenience comes a price: rapid antigen tests are not as sensitive as antibody tests or molecular (PCR) assays. You’re slightly more likely to get a false result with an antigen test.
Molecular Tests
Molecular COVID-19 tests look for the RNA component of the virus, as opposed to the proteins that antigen tests detect. The most common molecular test is called a polymerase chain reaction (PCR) test. The test utilizes a small sample of DNA that is then isolated and multiplied in a process called amplification. The virus is easier to detect when there’s plenty of genetic material to pore over! For this reason, these tests are commonly called nucleic acid amplification tests (NAATs).
The sample is generally collected with the same method (nasopharyngeal or oropharyngeal swab). When the test amplifies your genetic material, it attaches small strands of DNA to wherever it detects the viral genome. This process is repeated many times to create a larger sample of viral RNA.
Because PCR tests latch onto DNA and amplify the sample, they’re adept at catching even the smallest bits of viral RNA. Molecular tests, especially PCR tests, are currently the most reliable testing method on the market.
Antibody Tests
These are a little different! Instead of testing for current infection, an antibody test determines whether you had COVID-19 in the past. It detects antibodies present in your blood that only appear if you’ve gotten the virus already.
And because it’s a wholly different test, it requires a wholly different collection method: blood. If you were sick recently and suspect it was COVID-19, make an appointment with your doctor to get tested. The test, also called a serological test, requires a blood sample that is then sent off to a testing lab.
An antibody test will look for one of three different antibodies, called IgM, IgA, and IgG. The latter shows up in your system later on in the infection, and is the one most suspected of fighting off future infection. The best practice for getting an antibody test is to wait two weeks after your infection is gone. If you get tested too quickly, you risk a false negative result. This is because IgG shows up in your blood at the tail end of the infection, and if you test too quickly, you might not see it there.
A positive antibody test confirms that you have been exposed to the virus, but we don’t know yet how long those antibodies will last. It’s possible that IgG can make somebody immune to the virus, but maybe not permanently. Some studies have suggested that those antibodies lose effectiveness after a few months. Plus, with the spread of new variants of the virus, those antibodies may not be very effective in the first place.
If you plan on visiting folks outside your “bubble,” or if you’ve got travel plans on the books, make sure you get tested beforehand. You’ve got plenty of choices out there; it’s ultimately up to you. Rapid antigen tests are easy to perform and accessible to people who would rather take the test at home than visit a doctor’s office. Molecular PCR tests are currently the gold standard in COVID-19 testing, boasting nearly 100 percent accuracy. And if you’ve already been sick and don’t know if it was COVID-19, visit your doctor and take an antibody test. Slow the spread of the virus and hasten an end to the pandemic by ensuring that you are healthy when you go out in public. If you’re going to be in close contact with other people, you owe it to them as much as yourself to take a test. Understanding the different types of COVID-19 tests takes the mystery and uncertainty about the process. There’s no reason not to get tested!